Summary: Periodontal disease, often overlooked, plays a pivotal role in both oral health and systemic conditions in modern society. This article explores the multifaceted impacts of periodontal diseases from four crucial perspectives: their definitions and types, the connection between periodontal disease and systemic health, the role of prevention and treatment in contemporary care, and the challenges faced in public health awareness. By comprehensively understanding these aspects, we can appreciate the significance of maintaining periodontal health, which not only influences individual well-being but also public health as a whole.
1. Understanding the Types and Definitions
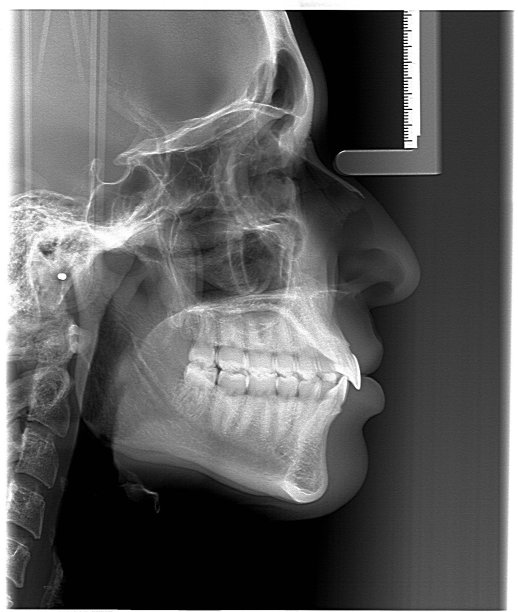
Periodontal disease encompasses a range of inflammatory conditions affecting the supporting structures of the teeth, including the gums and bones. The most common forms are gingivitis and periodontitis. Gingivitis is a mild form of periodontal disease characterized by inflammation and swelling of the gums, often reversible with proper oral hygiene. In contrast, periodontitis represents a more advanced stage that can lead to tooth loss and bone destruction.
The various forms of periodontal disease can be categorized based on severity and specific underlying causes, such as aggressive periodontitis and chronic periodontitis. Each type presents different symptoms and risk factors, necessitating tailored treatment approaches. Understanding these variations is vital for effective diagnosis and management, allowing healthcare providers to address each patient’s unique oral health needs.
Moreover, research has shown that genetic predisposition and environmental factors, such as tobacco use or diabetes, can influence the onset and progression of these diseases. Being aware of the different types of periodontal disease aids individuals in seeking timely intervention and has significant implications for overall health management.
2. Connections to Systemic Health
The link between periodontal disease and systemic health is increasingly recognized in medical discussions. Studies have evidenced associations between periodontal disease and various systemic diseases, including cardiovascular diseases, diabetes, and respiratory disorders. The inflammatory nature of periodontal disease can trigger systemic inflammatory responses, thus exacerbating conditions such as heart disease.
Diabetes, in particular, showcases a bidirectional relationship with periodontal disease—while uncontrolled diabetes increases the risk of periodontal infection, the presence of periodontal disease can make glycemic control more challenging. This connection emphasizes the compelling need for integrated healthcare approaches where dental and medical professionals collaborate.
Additionally, emerging evidence points to potential links between periodontal disease and adverse pregnancy outcomes. Pregnant women with periodontal complications may face an increased risk of preterm birth and low birth weight. Recognizing these associations is paramount as it highlights the importance of regular periodontal evaluations for women of childbearing age, ultimately benefiting maternal and fetal health.
3. Role of Prevention and Treatment
Preventing periodontal disease hinges on regular dental hygiene practices, including brushing, flossing, and routine dental check-ups. Education surrounding these practices is vital for altering public perceptions about oral care. Awareness campaigns can empower individuals to take charge of their oral health, thereby reducing the incidence of periodontal disease.
In practice, treatment modalities vary depending on the severity of the disease. Initial treatment may include non-surgical methods like scaling and root planing. However, advanced cases may necessitate surgical interventions. Dental professionals should emphasize the importance of routine follow-ups to monitor oral health and mitigate the risk of recurrence.
On a public health level, integrating preventive dental care into community health programs can be significantly beneficial. Strategies such as community screenings and educational workshops can raise awareness, especially in underserved populations where access to dental care is limited. By adopting a proactive approach, we can work toward reducing the prevalence of periodontal diseases on a larger scale.
4. Challenges in Public Health Awareness
One of the prominent challenges in addressing periodontal disease lies in the widespread lack of awareness about its potential consequences. Many individuals perceive oral health as separate from overall health, often disregarding signs of gum disease until they progress significantly. Overcoming this misconception requires concerted effort from both the dental community and broader public health initiatives.
Moreover, disparities in access to dental care can exacerbate the prevalence of periodontal disease, particularly among low-income communities. Limited insurance coverage for dental procedures further complicates access, underscoring the need for policy reforms aimed at making dental care more accessible to all populations.
Additionally, the impact of digital misinformation cannot be overlooked. While the internet has provided a wealth of information, it can also lead to the spread of myths regarding oral health practices. Combating misinformation through credible resources and promoting scientifically-backed information is crucial in fostering a healthier society.
Summary:
In conclusion, understanding periodontal disease is essential to appreciating its significant impact on both oral and systemic health. The interconnections highlighted throughout this article illustrate the importance of maintaining periodontal health, not only for individual well-being but also for public health outcomes. By enhancing awareness, promoting prevention, and addressing challenges in access to care, society can make strides toward a healthier future.
This article is compiled by Vickong Dental and the content is for reference only.


